Identification of key
In a study involving 13 hospitals in Spain and Italy, Dr. Enric Monreal and his team discovered that elevated serum neurofilament light chain (sNfL) levels, a marker of nerve cell damage, at the onset of multiple sclerosis (MS), can predict both relapse-associated worsening (RAW) and progression independent of relapse activity (PIRA) (1✔ ✔Trusted Source
Strategies to mitigate infection risks in MS therapies
).
Additionally, they found that serum glial fibrillary acidic protein (sGFAP) levels, which increase in the bloodstream due to central
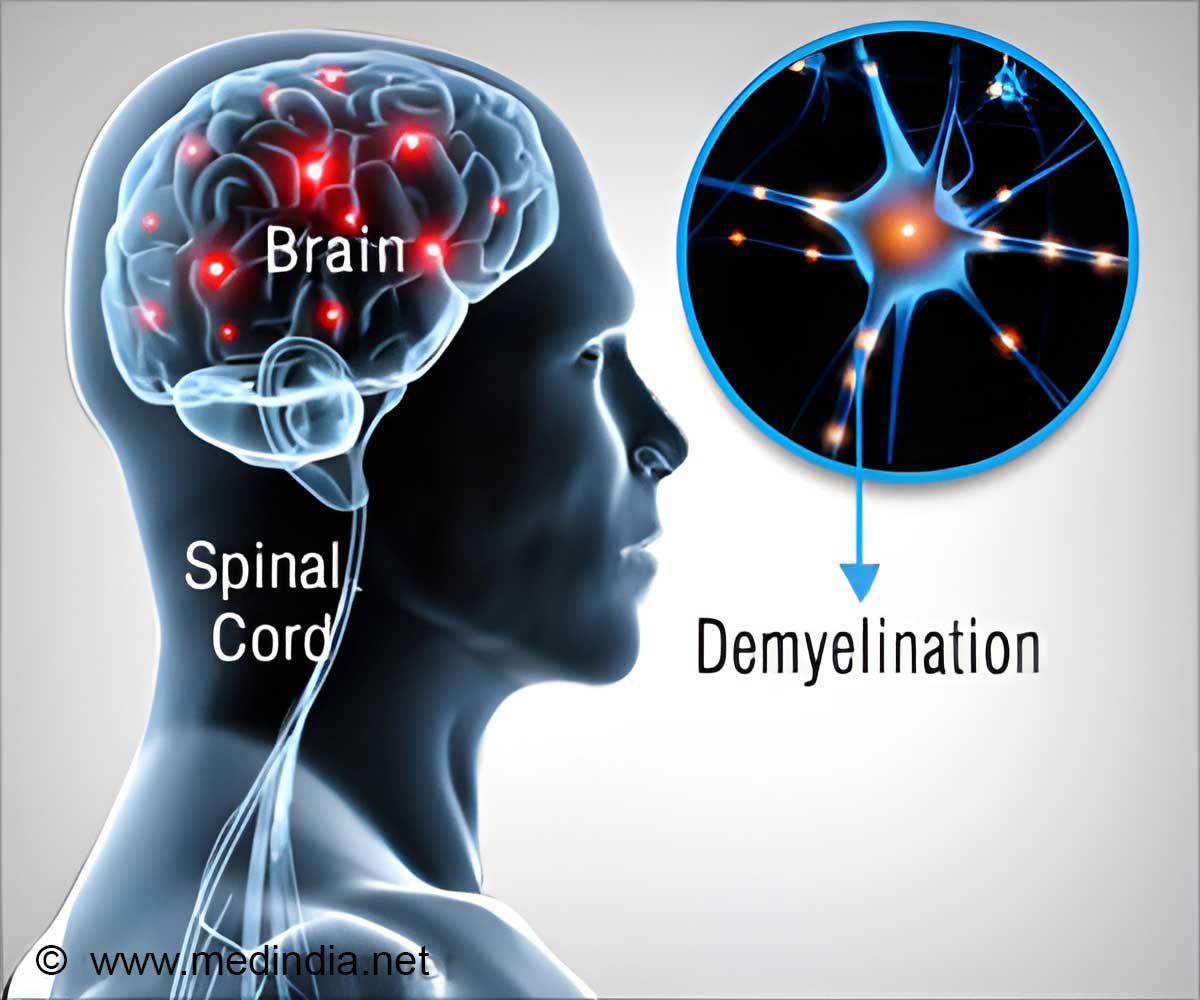
Critical Biomarkers for Multiple Sclerosis Identified
The researchers analyzed blood samples from 725 MS patients that were taken within a year of the disease’s onset for the study. Researchers evaluated the predictive usefulness of sNfL and sGFAP levels to predict RAW and PIRA using the Single Molecule Array (SIMOA) technology.
Important discoveries reveal a connection between elevated sNfL levels, a marker of
High-efficacy disease-modifying therapies (HE-DMTs), such as natalizumab, alemtuzumab, ocrelizumab, ritaximab, and ofatumumab, demonstrated notable improvements for patients with elevated sNfL levels who frequently did not respond well to conventional DMTs.
Conversely, patients exhibiting high levels of serum glial fibrillary acidic protein (sGFAP), which reflects localized inflammation caused by microglia in the central nervous system (CNS), faced an 86% increased risk of progression independent of relapse activity (PIRA).
Advertisement
Additionally, these patients had low serum neurofilament light chain (sNfL) levels and showed a lack of response to current disease-modifying therapies (DMTs).
Multiple Sclerosis Management Based on Biomarker Levels
Interestingly, while sGFAP is known to be associated with progression, high sNfL levels limited the ability of sGFAP to predict this outcome. Specifically, sGFAP values were predictive of PIRA only in patients with low sNfL levels.
Advertisement
“The identification of sNfL and sGFAP as predictive biomarkers allows us to tailor treatment strategies for MS patients more effectively,” says Dr. Monreal.
Patients with low levels of both biomarkers had a good prognosis and could be treated with injectable or oral DMTs. However, high sNfL levels indicate a need for HE-DMTs to prevent disability worsening, while patients with high sGFAP levels and low values of sNfL may require new therapeutic approaches.
These distinct pathways in MS have significant therapeutic implications, as current DMTs primarily target the peripheral adaptive
“The results of this study underscore the critical need for personalised treatment approaches to effectively manage the millions of people affected by MS worldwide, many of whom have a chronic disability that significantly impacts their quality of life,” says Dr. Monreal.
“By measuring both sNfL and sGFAP levels at disease onset, we gain valuable insights into the progression pathways of MS, enabling clinicians to identify the optimal patients for specific DMTs. This approach aims to prevent disability while avoiding unnecessary treatment-related risks for those at lower risk.”
Reference:
- Strategies to mitigate infection risks in MS therapies – (https:ectrims.eu/ectrims-spotlight-september-2024)
Source-Eurekalert